
Caries, Pulpitis and Apical Inflammation
This common bacterial infection, is characterized by the demineralization and destruction of tooth structure. And believe it or not, it is actually one of the most common diseases throughout the world.
Increases and decreases in the amount of caries in patients has been associated with widespread dietary changes that have occurred throughout time. Things that are associated with decreasing the amount of decay include the use of preventive measures, such as incorporating fluoride into the water supply, as well as using better oral hygiene methods.
In order for someone to develop cavities, there are four things that will be needed:
1. tooth surface- no tooth = no cavity!
2. cariogenic bacteria- need to have bacteria to cause the issue
3. dietary component (fermentable carbohydrates, such as sucrose)- Yum! Those sticky candies are the best!
4. time- to do the job on the teeth
When all four of these are present, cavities can develop. Other factors can also come into play. The shape of the teeth, the oral hygiene habits and the buffering capacity of the saliva are some examples.
Many, many years ago..... in a galaxy far, far away.....it was found that bacteria are found within the mouth and that these bacteria produce an acidic bacterial waste products as a by-product of living (yes, they "poop" it out). Unfortunately, it's these acidic waste products that dissolve tooth structure to cause demineralization and caries.
The main, cariogenic bacteria that's involved with the development and progression of dental caries is Streptococcus mutans. S. mutans initially collects on the teeth in plaque and will use fermentable sugars (mainly sucrose – table sugar, glucose and fructose) as a food source. As a by-product of metabolism, an acidic bacterial waste product is created. This acidic waste product will cause a localized decrease in pH, which in turn causes demineralization of the tooth structure.
So, why we tell patient's to brush after meals, three times a day, etc....? It's because if the acidic waste product is not removed or if there is a continuation of acidic waste product production (due to a continuous intake of sugars throughout the day), demineralization and caries is allowed to progress.
The process of demineralization is actually a dynamic process- in fact, demineralization of the tooth structure does occur, but remineralization of the tooth surface occurs as well. If the outer surface of the tooth dissolves (demineralization) for a few hours, remineralize of the surface occurs as the pH returns to normal (due to the buffering capacity of the saliva and the removal of the acids).
Another thing that is truly fascinating are the changes that are seen with respects to aging. As a person ages, caries is more commonly noted on the root surfaces of the teeth. Different bacteria are involved in root caries and the bacteria include Lactobacillus acidophilus, Actinomyces viscosus, Nocardia spp. and S. mutans.
So let's see how things are going so far with this material.....

 So, where do cavities occur on a tooth? The most common caries are fissural caries. More than 50% of all cavities in children and 90% of all cavities occur here. This type of cavity is most commonly detected using tactile (often with use of a dental explorer), visual (light and magnification), and radiographic means. Newer techniques for caries detection include the use of DIAGNOdent Caries Detector and fiber optic transillumination.
So, where do cavities occur on a tooth? The most common caries are fissural caries. More than 50% of all cavities in children and 90% of all cavities occur here. This type of cavity is most commonly detected using tactile (often with use of a dental explorer), visual (light and magnification), and radiographic means. Newer techniques for caries detection include the use of DIAGNOdent Caries Detector and fiber optic transillumination.

Cavities can also be found on the smooth surfaces of the teeth. Smooth surfaces include the interproximal and cervical surfaces, as well as the cusp tips. Caries in these areas are harder to detect, so x-rays (good ones of course....) come into play.

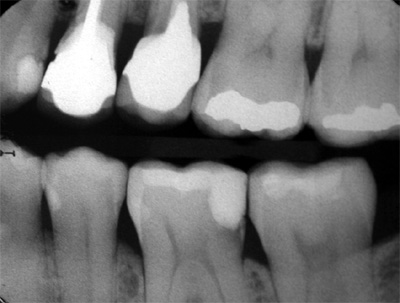
 Can you see the decay on this x-ray?
Can you see the decay on this x-ray?
If not do you need a hint?
Here are a few more clinical pictures for you to look at.
 Nice one at the cervical third of tooth #21. Talk about fun to try and restore when it extends below the gingiva.
Nice one at the cervical third of tooth #21. Talk about fun to try and restore when it extends below the gingiva.
 Here are a few small cavities on the cusp tips.
Here are a few small cavities on the cusp tips.

Ok, so now that you know where cavities are most commonly found, let's take a look at the different types of caries that patient's can have. Over the next two pages, we'll take a quick look at various types of caries. And yes, these pages are a little long. But that's only because of all the wonderful pictures I am trying to show you!
This normal type of decay occurs in most patients. It is a slowly progressing, continuous process that take's about 4 years for the cavity to pass through the enamel of the tooth.
This decay signifies advanced or severe decay that's present on multiple surfaces of teeth. It can be seen in those with xerostomia, poor oral hygiene, methamphetamine use (drug-induced dry mouth) and / or a large sugar intake.


This decay represents a type of rampant caries that may be seen when a patient undergoes head and neck radiation therapy. The patient is given high doses of radiation as a means of killing the cells of the cancer. Unfortunately, normal cells will die as well. If a salivary gland is directly in the field of radiation, the radiation will kill the normal cells of the salivary gland. A non-functioning salivary gland fails to create salivary secretions and xerostomia results. This xerostomia, along with a change in the oral microflora, a decrease in the cleansing abilities of the saliva and a change in the oral cavity's pH will all factor into the development of quickly progressing dental caries.


 Root caries is a quickly occurring decay process that is usually found when root surfaces have been exposed (due to gingival recession) and is most commonly noted on the facial surfaces. The root surface at the CEJ is more vulnerable to the demineralization process- cementum begins to demineralize at a pH of 6.7, whereas enamel's critical pH (where it begins to demineralize) is 5.5 (takes a lower pH is cause it's demineralization).
Root caries is a quickly occurring decay process that is usually found when root surfaces have been exposed (due to gingival recession) and is most commonly noted on the facial surfaces. The root surface at the CEJ is more vulnerable to the demineralization process- cementum begins to demineralize at a pH of 6.7, whereas enamel's critical pH (where it begins to demineralize) is 5.5 (takes a lower pH is cause it's demineralization).
As mentioned earlier, root caries is commonly seen in aging patients. As a patient ages, the number of medical conditions and the medications that they will be on will increase. Many medications cause xerostomia as a side effect. A reduction in salivary flow due to the physiology of aging and the patient exhibiting a decrease in manual dexterity will also come into play.

 This pattern of decay is found in young children and mainly involves the maxillary anterior teeth. It typically occurs when the child is allowed to fall asleep with a sweetened liquid in their bottle or feeding children sweetened liquids, multiple times during the day.
This pattern of decay is found in young children and mainly involves the maxillary anterior teeth. It typically occurs when the child is allowed to fall asleep with a sweetened liquid in their bottle or feeding children sweetened liquids, multiple times during the day.
So, why do you think nursing bottle caries is mostly seen involving the maxillary anterior teeth and not any of the mandibular teeth?
This type of caries will be found in locations that have been restored.
 Recurrent decay noted on the following:
Recurrent decay noted on the following:
#11 - distal
#14 - mesial
#19 - distal
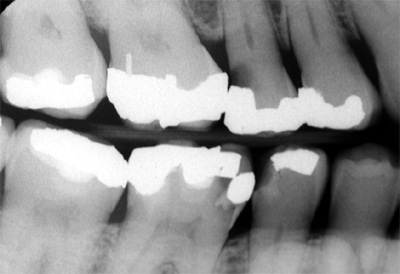 Recurrent decay noted on the following:
Recurrent decay noted on the following:
#4 - distal
#29 - distal
#30 - mesial
This term refers to decay that's just beginning and is at a location that has not previously experienced decay.
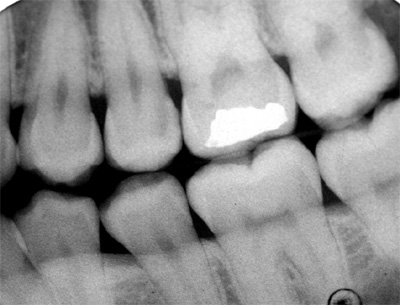
 So, can you see the incipient decay on this x-ray?
So, can you see the incipient decay on this x-ray?

 This type of decay describes a carious lesion on a tooth that was demineralized, but has undergone remineralization or caries that stopped due to the remineralization process. Arrested caries may be seen as dark, hardened areas within the tooth.
This type of decay describes a carious lesion on a tooth that was demineralized, but has undergone remineralization or caries that stopped due to the remineralization process. Arrested caries may be seen as dark, hardened areas within the tooth.
So, let's see how you are doing now!

In this section, we'll take a look at the steps that occur when a cavity develops.
 Wherever a cavity forms, the initial formation will begin with demineralization or decalcification of the enamel surface. An incipient lesion will form. Clinically, demineralization will be seen as a white spot and represents that a problem on the enamel surface is occurring. Areas of demineralization can remineralize to arrest (stop) the decay. The "decay" is actually reversible to this point, but the acids produced by Strep. mutans are neutralized. The easiest areas to see this finding are on the smooth surfaces of the teeth.
Wherever a cavity forms, the initial formation will begin with demineralization or decalcification of the enamel surface. An incipient lesion will form. Clinically, demineralization will be seen as a white spot and represents that a problem on the enamel surface is occurring. Areas of demineralization can remineralize to arrest (stop) the decay. The "decay" is actually reversible to this point, but the acids produced by Strep. mutans are neutralized. The easiest areas to see this finding are on the smooth surfaces of the teeth.
 The same thing occurs on the interproximal surfaces, but is harder to visualize clinically. That's why we rely on radiographs. Take a look at the distal surface of tooth #29. This shows an incipient lesion that is within the enamel and getting closer to the DEJ.
The same thing occurs on the interproximal surfaces, but is harder to visualize clinically. That's why we rely on radiographs. Take a look at the distal surface of tooth #29. This shows an incipient lesion that is within the enamel and getting closer to the DEJ.
 If an incipient lesion is not treated, the decay progresses to destroy the enamel to the DEJ.
If an incipient lesion is not treated, the decay progresses to destroy the enamel to the DEJ.
The x-ray to the right shows an untreated incipient lesion on the distal of tooth #19. This interproximal lesion has a characteristic triangular shape with the apex (smallest point) going towards the DEJ. Once the lesion reaches the DEJ, it will spread laterally long the DEJ. If left untreated, the dentin will become demineralized.
In time, the decay advances towards the pulp if left untreated.
 This photo shows a good amount of decay on the facial surface of tooth #6. The chalky white area on the facial surface is demineralized enamel. The brownish colored area is demineralized dentin (cavity is within the dentin).
This photo shows a good amount of decay on the facial surface of tooth #6. The chalky white area on the facial surface is demineralized enamel. The brownish colored area is demineralized dentin (cavity is within the dentin).
Tooth #7 also shows demineralization and decay on the facial surface.

The photo to the right is showing the inside of a tooth during a restorative procedure. An occlusal amalgam was removed (due to recurrent decay) and the decay removed. The cavity was deep and extended towards the pulp of the tooth. If you look closely, you can see that the deepest portion of the preparation floor is red in color. The red color is telling you that the pulp is very close. Look even closer- do you see the small red dot that is closer to the buccal side of the tooth? That's a pulp horn that's showing.

 Areas of demineralization will show a color change and will appear chalky white. These areas can also stain and make the area appear brown or black.
Areas of demineralization will show a color change and will appear chalky white. These areas can also stain and make the area appear brown or black.
 In some cases, it's possible to see decay interproximally. These areas will exhibit a discoloration of the marginal ridge. The clinical photo to the right shows discoloration on the distal surface of tooth #13. A cavity is verified to be present when a bitewing is taken.
In some cases, it's possible to see decay interproximally. These areas will exhibit a discoloration of the marginal ridge. The clinical photo to the right shows discoloration on the distal surface of tooth #13. A cavity is verified to be present when a bitewing is taken.

 If demineralization continues, a loss of enamel / hard tissue will occur. This loss of enamel creates an undermining of the outer surface and is called cavitation. It's almost like digging a tunnel underneath the ground. You are in the tunnel and have a small area of dirt / ground above you. Yes, if someone walks on the ground above the tunnel, the tunnel colapses. That's what happens in a cavity. The outer shell of enamel will colapse and a hole becomes evident.
If demineralization continues, a loss of enamel / hard tissue will occur. This loss of enamel creates an undermining of the outer surface and is called cavitation. It's almost like digging a tunnel underneath the ground. You are in the tunnel and have a small area of dirt / ground above you. Yes, if someone walks on the ground above the tunnel, the tunnel colapses. That's what happens in a cavity. The outer shell of enamel will colapse and a hole becomes evident.
One of the most common ways to check or verify areas of decay is through the use of an explorer. Using the tine of the explorer, the enamel surface will be checked for areas of stickiness (enamel softness).
If a patient has a cavity, they may experience some sensitivity. Like everything in life, patients can have variations in what they experience.
Some of the symptoms that a patient may notice include sensitivity to sweets, hot or cold.
Ok, so let's see how things are going again....

Pulpitis is defined as inflammation of the pulpal tissues. It can occur when decay is left untreated or if there is an insult or injury to the tooth. In either case, the tooth exhibits some sort of tooth sensitivity.
There are two types of pulpitis:

 Yes, as you think..... necrosis tells you that something is dead and pulpal necrosis is telling you that the pulp has died. When the pulp of a tooth dies, the tooth is termed non-vital. Dead teeth or non-vital teeth are asymptomatic and therefore cause no discomfort to the the patient. In some cases, a dead tooth can be seen clinical with a discolored crown. In these cases, a periapical radiograph will be taken.
Yes, as you think..... necrosis tells you that something is dead and pulpal necrosis is telling you that the pulp has died. When the pulp of a tooth dies, the tooth is termed non-vital. Dead teeth or non-vital teeth are asymptomatic and therefore cause no discomfort to the the patient. In some cases, a dead tooth can be seen clinical with a discolored crown. In these cases, a periapical radiograph will be taken.
When you think about an abscess, do you think about a painful situation? This is true for some cases, but not true for all.
The term periapical abscess refers to the acute phase of an infection that spreads from a non-vital tooth through the apical foramen and into the alveolar bone. The periapical region is abscessed and will contain WBCs and cellular debris. This infection can also spread into the adjacent soft tissues.
Clinical findings associated with a periapical abscess:
 These terms refer to a chronic abscess associated with a tooth and are the result of chronic periapical inflammation.
These terms refer to a chronic abscess associated with a tooth and are the result of chronic periapical inflammation.
Clinical findings associated with a granuloma:

Granulomas may also be seen clinically. Here is a patient case (clinical / x-ray).

So, let's see if you have been learning anything.....

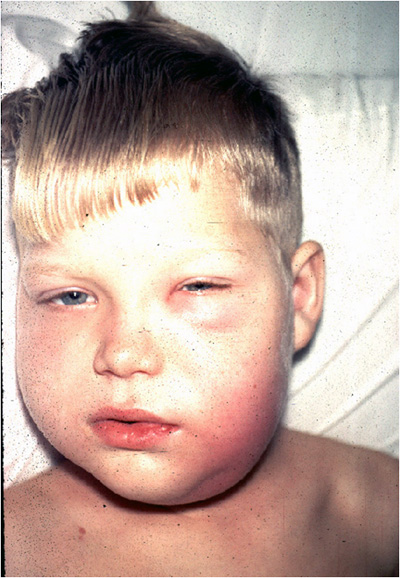
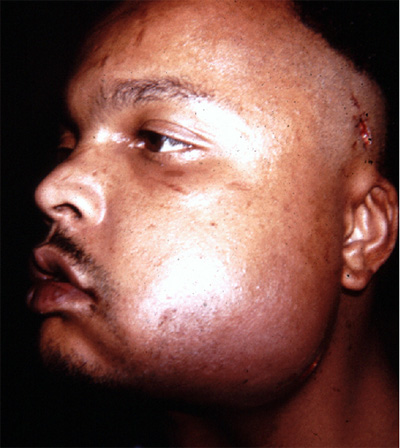
Cellulitis is defined as a diffuse infection of connective tissue with severe inflammation of dermal and subcutaneous layers of the skin. What this is telling you is that the infection that was once localized, has now spread into the adjacent soft tissue.
Cellulitis can be seen in any part of the body, but when we look at cellulitis with a dental origin. Dental related cellulitis typically involves abscessed teeth and impacted third molars.
Clinical findings associated with cellulitis:
Here are a few clinical pictures of dental related cellulitis.

Let's now give you a few more terms that relate to dental infections. A sinus tract represents an abnormal channel leading from within one structure to the surface of the skin. A fistula is the opening of the sinus tract on the outside of the skin. Think about the following scenario- Imagine a small tube going from the apex of tooth #20 to the outside of the face (skin). The tube represents the sinus tract and the outside opening on the face represents the fistula.
Here you can see two examples of fistulas. I especially like the draining one!


 Ludwig's angina is a serious, potentially life-threatening type of cellulitis that involves inflammation of the tissues of the floor of the mouth and underside of the tongue. It most often occurs in adults with concomitant dental infections and is frequently associated with abscessed teeth, infected mandibular molars and/or pericoronitis.
Ludwig's angina is a serious, potentially life-threatening type of cellulitis that involves inflammation of the tissues of the floor of the mouth and underside of the tongue. It most often occurs in adults with concomitant dental infections and is frequently associated with abscessed teeth, infected mandibular molars and/or pericoronitis.
The cause of Ludwig's angina is usually bacterial in nature and typically involves Actinomyces israelii and other actinomyces species. Since the advent of antibiotics, Ludwig's angina has become a rare disease.
Symptoms of Ludwig's angina include swelling, pain, raising of the tongue, swelling of the neck and the tissues of the submandibular and sublingual spaces, malaise, fever, dysphagia (difficulty swallowing) and, in severe cases, stridor or difficulty breathing. Airway compromise is a serious complication.
 Cavernous sinus thrombosis is a very rare, typically septic, with a poor prognosis, thrombosis of the cavernous sinus, usually caused by bacterial sinusitis. Symptoms and signs include pain, proptosis, ophthalmoplegia, vision loss, papilledema, and fever.
Cavernous sinus thrombosis is a very rare, typically septic, with a poor prognosis, thrombosis of the cavernous sinus, usually caused by bacterial sinusitis. Symptoms and signs include pain, proptosis, ophthalmoplegia, vision loss, papilledema, and fever.
Don't worry about memorizing the details of each of these severe complications. Just be aware of what Ludwig's angina and Cavernous sinus thrombosis are.
And yes, one more question.....
